Curative surgical treatment
![]() We
have just seen what was used yesterday. A few surgeons justly
continue to use this stable material which has proved its excellent
efficacy.
We
have just seen what was used yesterday. A few surgeons justly
continue to use this stable material which has proved its excellent
efficacy.
![]() Most
traumatology surgeons have started using another type of equipment, screw-plates.
Since bone loss, linked to osteoporosis, weakens the neck of the femur,
they prefer to embed the two largest fragments one into the other. They
do not attempt to stabilise the secondary fragments, nor do they bother
about replenishing the lost bone which, in the neck of the femur was definitively
compressed by the fall, leaving a hole which is even bigger when the osteoporosis
is advanced.
Most
traumatology surgeons have started using another type of equipment, screw-plates.
Since bone loss, linked to osteoporosis, weakens the neck of the femur,
they prefer to embed the two largest fragments one into the other. They
do not attempt to stabilise the secondary fragments, nor do they bother
about replenishing the lost bone which, in the neck of the femur was definitively
compressed by the fall, leaving a hole which is even bigger when the osteoporosis
is advanced.
![]() This
classic surgical equipment is therefore designed to hold the two main
fragments of a fractured femoral neck in the right position. It consists
of two metal parts: the first (cephalic screw) is screwed into the head
of the femur; the second (screw-plate) is screwed to the body of the bone.
These are held together by the gun. This is welded to the plate at an
angle of 130° equivalent to that of the femoral neck.
This
classic surgical equipment is therefore designed to hold the two main
fragments of a fractured femoral neck in the right position. It consists
of two metal parts: the first (cephalic screw) is screwed into the head
of the femur; the second (screw-plate) is screwed to the body of the bone.
These are held together by the gun. This is welded to the plate at an
angle of 130° equivalent to that of the femoral neck.
![]() Although
the great advantage of this equipment is to avoid exceptional cases of
migration outside the head, its major disadvantage is that you cannot
control the degree of penetration of the fragments into each other. A
minimum penetration of 10 mm would not have any great consequence but
the same does not apply if it reaches 15 or 20 mm and sometimes more.
Although
the great advantage of this equipment is to avoid exceptional cases of
migration outside the head, its major disadvantage is that you cannot
control the degree of penetration of the fragments into each other. A
minimum penetration of 10 mm would not have any great consequence but
the same does not apply if it reaches 15 or 20 mm and sometimes more.
![]() To
stabilise a complex fracture (more than two fragments), all the pieces
of broken bone must be reconstructed and held together. This stabilisation
takes place in two stages.
To
stabilise a complex fracture (more than two fragments), all the pieces
of broken bone must be reconstructed and held together. This stabilisation
takes place in two stages.
How to restore the anatomy of a complex fracture: current technique: screw plate and cables
![]() Initially,
the type of fracture must be defined by analysing the main and secondary
lines.
Initially,
the type of fracture must be defined by analysing the main and secondary
lines.
see following article
Y. Cirotteau Boyd H.B. and Griffin L.L. classification :
A refinement proposal. Eur J Orthop Surg Traumatol (2002) 12 : 152-157
For further information: modified classification of osteoporotic trochanter fractures (available in french only)
![]() Secondly,
the main fracture must be reduced (joining fragments 1 and 2) as well
as secondary lines. This can be done using a stabilised screw plate to
hold the main fracture line and cables to maintain the secondaries.
Secondly,
the main fracture must be reduced (joining fragments 1 and 2) as well
as secondary lines. This can be done using a stabilised screw plate to
hold the main fracture line and cables to maintain the secondaries.
![]() In
addition to the fact that limping in these cases is inevitable for a long
time, a state of spinal column imbalance will also be inevitable in the
medium or long term. We can always convince ourselves that this is not
very important for someone at the end of their life, but this is not our
opinion. And for a younger person (60-65 years old) I'm not certain he
or she would agree.
In
addition to the fact that limping in these cases is inevitable for a long
time, a state of spinal column imbalance will also be inevitable in the
medium or long term. We can always convince ourselves that this is not
very important for someone at the end of their life, but this is not our
opinion. And for a younger person (60-65 years old) I'm not certain he
or she would agree.
For older people, how can we accept the idea of further reducing their
falling muscular strength, which they need in order to stand up, walk
and/or go up and down stairs? This is not a serious approach.
![]() It
seems quite legitimate and justified, if there are secondary fractures
as well as the main two fracture fragments, to treat them with the same
amount of attention. This is the intention of the cables. It may be necessary
to fix the greater or lesser trochanter or both. Here are a few examples.
It
seems quite legitimate and justified, if there are secondary fractures
as well as the main two fracture fragments, to treat them with the same
amount of attention. This is the intention of the cables. It may be necessary
to fix the greater or lesser trochanter or both. Here are a few examples.
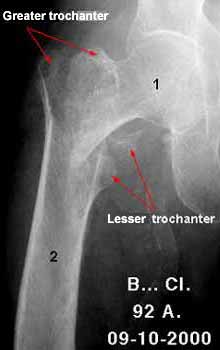 Fractured hip (front view) Main line and greater trochanter |
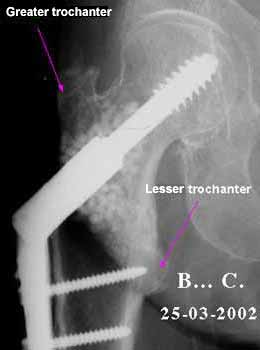 Consolidated hip (front view) |
 Consolidated hip (side view) Consolidation of main line and greater trochanter |
 Fractured hip (front view) Main line and greater trochanter |
 Post-operative (front view) Stabilisation of main line and greater trochanter |
 Post-operative (side view) |
 Fractured hip (front view) Main line and greater and lesser trochanter |
 Immediately post-operative (front view) Stabilisation of main line and both trochanters |
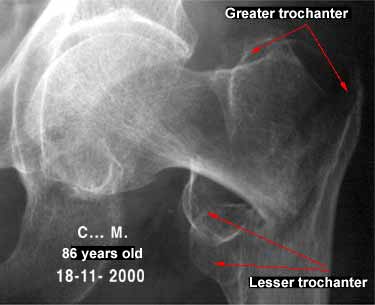 Fractured hip (front view) Main line and greater and lesser trochanter (two fragments) |
 Consolidated hip (front view) |
For further information... the surgical technique (available in french only)
What is the benefit to the patient?
![]() In
the immediate there is a distinct reduction in pain. It is curious to
note that although all traumatologists agree that the best antalgic (treatment
against pain), in cases of fracture, is firstly immobilisation, yet, as
soon as femoral neck fractures are concerned, they "forget"
this basic principle!
In
the immediate there is a distinct reduction in pain. It is curious to
note that although all traumatologists agree that the best antalgic (treatment
against pain), in cases of fracture, is firstly immobilisation, yet, as
soon as femoral neck fractures are concerned, they "forget"
this basic principle!
![]() Nevertheless, since
time immemorial, fractured members were immobilised by splints: then plaster
and resin were invented, osteosynthesis (fixing with metal components
consisting of screws, nails, plates etc.).
Nevertheless, since
time immemorial, fractured members were immobilised by splints: then plaster
and resin were invented, osteosynthesis (fixing with metal components
consisting of screws, nails, plates etc.).
The more stable the fracture the more the pieces are prevented
from moving with respect to each other the less painful it is.
It is clear that the better the assembly fixes the broken pieces and holds
them together, the more stable it is from a purely mechanical viewpoint.
![]() If we take the example
of a chair with a broken leg, it is easy to imagine that you can only
sit on it if
If we take the example
of a chair with a broken leg, it is easy to imagine that you can only
sit on it if
the leg is solid. To obtain this you can use glue, plugs, screws or nails.
Sometimes, it's true, it's better to make a new leg. Alas, this is not
possible for us!
In the same way that we would not hesitate to sit on a strong chair, so
the patient who is not in pain and feels stable will not hesitate to put
his weight on the broken leg. Everyone knows that it's impossible to ask
an elderly person to hop on the one reliable leg.
![]() This is the all-or-nothing
law. There is no choice. Either you fix it all or you fix a little and,
in this case, it's as if nothing is fixed. Incidentally, leaving a 75
or 80 year old person in bed for 6 weeks is a confession of impotence.
Everything must be done for the person suffering the fracture to be on
his feet as quickly as possible. Fractures in the elderly should no longer
be a source of fear for the patient or the trauma surgeon.
This is the all-or-nothing
law. There is no choice. Either you fix it all or you fix a little and,
in this case, it's as if nothing is fixed. Incidentally, leaving a 75
or 80 year old person in bed for 6 weeks is a confession of impotence.
Everything must be done for the person suffering the fracture to be on
his feet as quickly as possible. Fractures in the elderly should no longer
be a source of fear for the patient or the trauma surgeon.
What happens several weeks later?
![]() Putting
weight on a bone is essential for its good health. Astronauts who remain
in space for a long time, suffer from skeletal disorders among
others. Bones need to bear weight if they are to remain in good health.
If you can put weight on a repaired bone it will be in the best condition
for healing.
Putting
weight on a bone is essential for its good health. Astronauts who remain
in space for a long time, suffer from skeletal disorders among
others. Bones need to bear weight if they are to remain in good health.
If you can put weight on a repaired bone it will be in the best condition
for healing.
If it is also provided with the elements necessary for its good health,
it will consolidate twice as fast (in 50% of cases) or in two months (in
75% of cases) i.e. 1/3 less time than with classic treatment, the average
duration of which is three and sometimes four months.
![]() At
present, the classic treatment consists of only treating the main line,
neglecting secondary lines when they are present and totally ignoring
the cause.
At
present, the classic treatment consists of only treating the main line,
neglecting secondary lines when they are present and totally ignoring
the cause.
Does this mean we are not interested in caring for the elderly? Those
responsible for the "Bone and Joint Decade" meet in huge intercontinental
palaces, have Royal, Papal and Republican patrons, discourse on the possibility
of holding the next conference if possible on some far-flung
isle.
![]() If you are curious
enough to attend a few conferences, you see, immediately on arriving,
gigantic panels displaying the name of some product or other which is
said to be excellent against bone loss. Trauma surgeons will soon be out
of a job. Thank goodness it's not here yet in so far as there
are still surgeons! That's another story.
If you are curious
enough to attend a few conferences, you see, immediately on arriving,
gigantic panels displaying the name of some product or other which is
said to be excellent against bone loss. Trauma surgeons will soon be out
of a job. Thank goodness it's not here yet in so far as there
are still surgeons! That's another story.
![]() Without getting
into a stupid argument, we must acknowledge that these huge events do
make you smile a bit. It would be interesting to ask a member of the audience
what he remembers from a speech made by a speaker certain of the essential
role played by some kind of ribosome on the dextrorotatory version of
an alkylated aromatic molecule in the presence of a tartric acid bound
to transgenic messenger RNA! You will have understood that this miserable
conference had no other purpose than to show how the mean level of basic
medicine such as traumatology cannot follow such high-flown
science. Only a few initiates of the inner circle are capable of following
what is hidden behind these formulae. I want to spare the brave reader
who has followed me this far. All this to say: "what about the broken
patient?"
Without getting
into a stupid argument, we must acknowledge that these huge events do
make you smile a bit. It would be interesting to ask a member of the audience
what he remembers from a speech made by a speaker certain of the essential
role played by some kind of ribosome on the dextrorotatory version of
an alkylated aromatic molecule in the presence of a tartric acid bound
to transgenic messenger RNA! You will have understood that this miserable
conference had no other purpose than to show how the mean level of basic
medicine such as traumatology cannot follow such high-flown
science. Only a few initiates of the inner circle are capable of following
what is hidden behind these formulae. I want to spare the brave reader
who has followed me this far. All this to say: "what about the broken
patient?"
![]() All this is also
good if as we saw above there is some bony support (the
rails) and the wagons (the vessels) to transport the drugs (Replacement
hormones and diphosphonates) and workers (bone cells) to the right place
so that they can work together. We shall not go into more intracellular
detail because we are discussing surgical osteoporosis here.
All this is also
good if as we saw above there is some bony support (the
rails) and the wagons (the vessels) to transport the drugs (Replacement
hormones and diphosphonates) and workers (bone cells) to the right place
so that they can work together. We shall not go into more intracellular
detail because we are discussing surgical osteoporosis here.
![]() We shall simply
say that one reaches a stage where old age being a shipwreck
it seems that everything has been said but there is still a captain on
board for how long? That's another problem.
We shall simply
say that one reaches a stage where old age being a shipwreck
it seems that everything has been said but there is still a captain on
board for how long? That's another problem.
He must make sure that all breaches in the hull (the container) are filled
by using biomaterial (in this case natural coral) then, he will rebuild
the bridge and passageways if necessary (the content: the broken
pieces). What captain would agree to sail a boat only half repaired? What
wise man would risk his life on such a frail craft? Don't our little grannies
deserve more than a half-repaired boat?
![]() Must we ask the
fearful question of whether we really want to do something for our "old
folks"? How charming it is to see the solicitude of our elected representative
for old people before the elections. And when they break a hip, when it's
too hot, who will go and see them? Who looks after them? Hospital emergency
departments, charity organisations and, if there are still any around,
trauma surgeons. The whole problem is to know whether or not they have
the financial and technical resources to do the job properly.
Must we ask the
fearful question of whether we really want to do something for our "old
folks"? How charming it is to see the solicitude of our elected representative
for old people before the elections. And when they break a hip, when it's
too hot, who will go and see them? Who looks after them? Hospital emergency
departments, charity organisations and, if there are still any around,
trauma surgeons. The whole problem is to know whether or not they have
the financial and technical resources to do the job properly.
![]() For charity organisations
the question doesn't arise because they are wonderful volunteers. I pay
tribute to them here. Alas, without denying the exceptional qualities
of their good hearts devotion, compassion, availability, generosity
they don't give good service to the State which relies on them
to attenuate its inadequacies. Since it intends to manage Health
Soviet fashion it should take charge with the same advantages
for everyone. Post-war French Medicine was the best in the World. Today
it is in the process of becoming one of the worst, due to lack of resources
(like England and the Eastern Bloc) in spite of the recent appreciation
inaccurate by certain leftist ministers. We are not yet
talking about the professional quality of those providing this care.
For charity organisations
the question doesn't arise because they are wonderful volunteers. I pay
tribute to them here. Alas, without denying the exceptional qualities
of their good hearts devotion, compassion, availability, generosity
they don't give good service to the State which relies on them
to attenuate its inadequacies. Since it intends to manage Health
Soviet fashion it should take charge with the same advantages
for everyone. Post-war French Medicine was the best in the World. Today
it is in the process of becoming one of the worst, due to lack of resources
(like England and the Eastern Bloc) in spite of the recent appreciation
inaccurate by certain leftist ministers. We are not yet
talking about the professional quality of those providing this care.
![]() Casualty staff are
complaining loudly and their voices are beginning to be heard. They must
continue. They must demand more premises, greater competence in their
physicians, more rest for these girls and boys who are overworked and
literally exhausted after a night on duty.
Casualty staff are
complaining loudly and their voices are beginning to be heard. They must
continue. They must demand more premises, greater competence in their
physicians, more rest for these girls and boys who are overworked and
literally exhausted after a night on duty.
![]() In the opinion of
traumatologists, it is the State. Since 1968, the situation in public
hospitals, with a few exceptions, has deteriorated dramatically. The A.R.H
(Agence Rιgionale d'Hospitalisation Regional hospitalisation
agency) the director holding the rank of superprefect
has full power to close hospital beds throughout the land according to
criteria which he alone can define! When the decision is made there is
nothing to be done. Unless the population, fed up with penalising decisions,
decides, as they did in Millau to take peaceful action and use
the Media to voice their complaints. Bravo.
In the opinion of
traumatologists, it is the State. Since 1968, the situation in public
hospitals, with a few exceptions, has deteriorated dramatically. The A.R.H
(Agence Rιgionale d'Hospitalisation Regional hospitalisation
agency) the director holding the rank of superprefect
has full power to close hospital beds throughout the land according to
criteria which he alone can define! When the decision is made there is
nothing to be done. Unless the population, fed up with penalising decisions,
decides, as they did in Millau to take peaceful action and use
the Media to voice their complaints. Bravo.
In conclusion:
![]() Curative
surgical treatment of a fracture caused by osteoporosis should be treated
with the greatest care by all health partners: traumatologists and social
partners. Traumatologists should pay more attention to rebuilding the
bone as a whole. Social partners should provide them with the resources
to do so.
Curative
surgical treatment of a fracture caused by osteoporosis should be treated
with the greatest care by all health partners: traumatologists and social
partners. Traumatologists should pay more attention to rebuilding the
bone as a whole. Social partners should provide them with the resources
to do so.
![]() A new philosophy
is not always easy to admit. Once again it is good to remember that when
it concerns the well-being of a large number, the whole group benefits.
A new philosophy
is not always easy to admit. Once again it is good to remember that when
it concerns the well-being of a large number, the whole group benefits.
| Last page |