Preventive surgical treatment
4 - Mrs L.M.G.
![]() She
is an adorable little granny (1m48), 85 years old. She fractured her left
hip. Secondary arthrosis meant the ablation of material.
She
is an adorable little granny (1m48), 85 years old. She fractured her left
hip. Secondary arthrosis meant the ablation of material.
 |
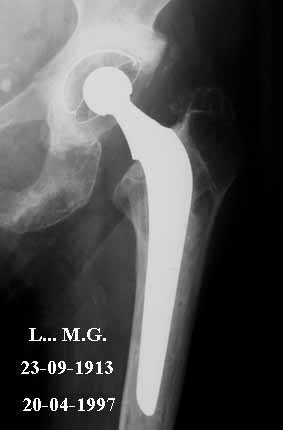 |
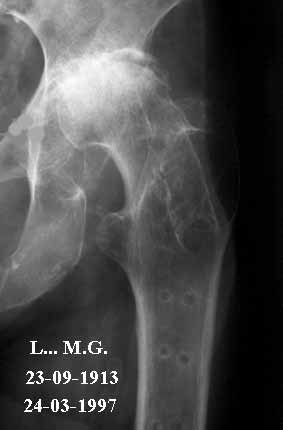
| Left hip: severely handicapping coxarthrosis | Sir J. Charnely's total prosthesis |
![]() This
arthrosis had intensified to the extent that she could no longer leave
her home because of the pain. She is very active and alert and suffered
a great deal from this situation. The solution – for the left hip
– was clearly a full prosthesis.
This
arthrosis had intensified to the extent that she could no longer leave
her home because of the pain. She is very active and alert and suffered
a great deal from this situation. The solution – for the left hip
– was clearly a full prosthesis.
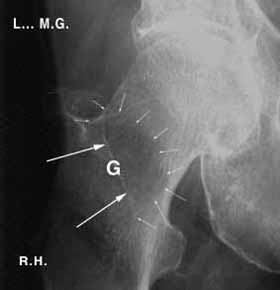
![]() On
looking carefully at the X-ray of the opposite hip, a large hole can be
seen, the site and volume of which affect the entire upper part of the
femur. Not only are the bone trabeculae affected, but you can see through
to the back of the bone. This part is usually invisible because of the
density of normal bone.
On
looking carefully at the X-ray of the opposite hip, a large hole can be
seen, the site and volume of which affect the entire upper part of the
femur. Not only are the bone trabeculae affected, but you can see through
to the back of the bone. This part is usually invisible because of the
density of normal bone.
 |
 |
| Right hip: major osteoporosis | Osteoscopy of the right hip |
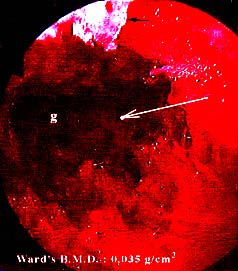
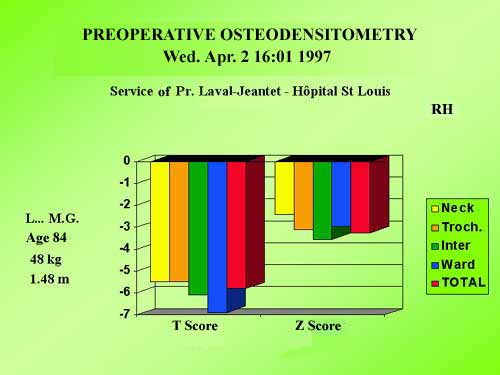
![]() Bone
densitometry was requested. It confirmed the severity of the osteoporosis
because the BMD in the affected part was only a few dozen mg/cm²
(normally several hundred).
Bone
densitometry was requested. It confirmed the severity of the osteoporosis
because the BMD in the affected part was only a few dozen mg/cm²
(normally several hundred).
![]() It is clear that under such conditions of bone fragility, at the slightest
fall this patient was likely to suffer a fracture. Remember that the risk
of fracture is all the more serious when densitometric loss is severe.
Even worse, even if she didn't fall there was still a very high risk that
a fatigue fracture could occur simply during a longer than usual walk.
It is clear that under such conditions of bone fragility, at the slightest
fall this patient was likely to suffer a fracture. Remember that the risk
of fracture is all the more serious when densitometric loss is severe.
Even worse, even if she didn't fall there was still a very high risk that
a fatigue fracture could occur simply during a longer than usual walk.
![]() For
example: you can break a thin metal wall with a sharp blow against a harder
surface. This same wall can also be bent by bending it and moving it backwards
and forwards. After several flexions the wall will suddenly break. This
is a fatigue fracture.
For
example: you can break a thin metal wall with a sharp blow against a harder
surface. This same wall can also be bent by bending it and moving it backwards
and forwards. After several flexions the wall will suddenly break. This
is a fatigue fracture.
![]() Installation
of the full prosthesis would encourage the patient to become fully active
once more because she would no longer be in pain. She would be able to
go shopping, visit exhibitions, go to the cinema, use public transport,
etc. Knowing that the other hip could be fractured at any moment, do we
have the right to do nothing? Wait for the fracture with our arms crossed?
Installation
of the full prosthesis would encourage the patient to become fully active
once more because she would no longer be in pain. She would be able to
go shopping, visit exhibitions, go to the cinema, use public transport,
etc. Knowing that the other hip could be fractured at any moment, do we
have the right to do nothing? Wait for the fracture with our arms crossed?
![]() In
our opinion, we have neither the moral nor the scientific right to leave
it to chance when we know that the inevitable will happen sooner or later.
When you are 85 years old you no longer have much life left ahead of you:
later can arrive pretty soon.
In
our opinion, we have neither the moral nor the scientific right to leave
it to chance when we know that the inevitable will happen sooner or later.
When you are 85 years old you no longer have much life left ahead of you:
later can arrive pretty soon.
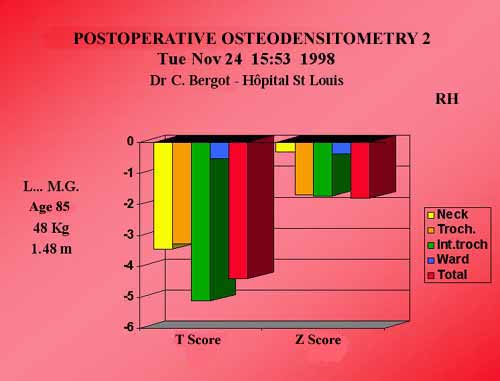
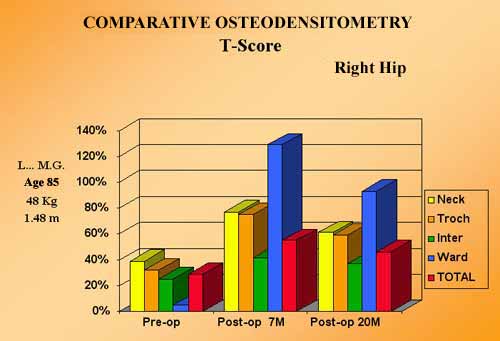
![]() During
a family reunion, the reasons for preventive treatment were explained.
The family accepted the conclusions and a filling-graft was performed.
X-rays show the gradual disappearance of the natural coral. Two densitometries
were performed 7 and 20 months later.
During
a family reunion, the reasons for preventive treatment were explained.
The family accepted the conclusions and a filling-graft was performed.
X-rays show the gradual disappearance of the natural coral. Two densitometries
were performed 7 and 20 months later.
|
|
![]() They
show major reconstruction of the bone structure with a 20% increase in
the high-risk zone and filling of the hollow centre of the bone with almost
100% mineralisation.
They
show major reconstruction of the bone structure with a 20% increase in
the high-risk zone and filling of the hollow centre of the bone with almost
100% mineralisation.
![]() Clinically,
two and a half years after the graft, this patient could leave her home
again, did her shopping with her daughter and visited the supermarket.
She danced at Christmas. At her examination she had gained 15 kilos and
was in good health. Mentally, her life had been transformed.
Clinically,
two and a half years after the graft, this patient could leave her home
again, did her shopping with her daughter and visited the supermarket.
She danced at Christmas. At her examination she had gained 15 kilos and
was in good health. Mentally, her life had been transformed.
![]() The
graft of biomaterial, restoring the strength of her bone structures allowed
this patient to regain full autonomy and overcome the fear of falling
suffered by all patients who have had a fractured hip. This fear closes
them even more within their walls in an atmosphere of increasing anxiety
and isolation.
The
graft of biomaterial, restoring the strength of her bone structures allowed
this patient to regain full autonomy and overcome the fear of falling
suffered by all patients who have had a fractured hip. This fear closes
them even more within their walls in an atmosphere of increasing anxiety
and isolation.
![]() The
feeling of freedom inspired by being able to stand up is a major factor
for the well-being of everyone, but particularly for the elderly, as long
as their legitimate fear of fracturing a hip can be conquered with, under
present conditions of classic treatment, the possibility of more or less
severe sequelae during the time they have left to live.
The
feeling of freedom inspired by being able to stand up is a major factor
for the well-being of everyone, but particularly for the elderly, as long
as their legitimate fear of fracturing a hip can be conquered with, under
present conditions of classic treatment, the possibility of more or less
severe sequelae during the time they have left to live.
| Previous page |

